Dry eye syndrome is a condition affecting millions of peo- ple worldwide. It occurs when the eyes fail to produce enough tears or when the tears evaporate too quickly. It can often lead to discomfort and potential damage to the eye's surface. This condition can arise from factors such as aging, prolonged screen time, low humidity, fans and wind, and underlying medical issues. Left untreated, dry eyes can interfere with daily activities like reading, driving, wearing contact lenses and cosmetics, and using digital devices. The good news is that your dry eye specialist has many new tools to diagnose and treat this common problem.
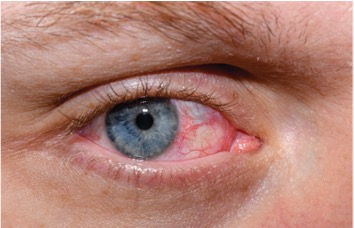
The primary function of tears is to lubricate and protect the eyes. Tears con- sist of three layers: the oily layer, which prevents evaporation; the watery layer, which provides hydration; and the mucous layer, which ensures the tears spread evenly across the eye surface. An imbalance in any of these lay- ers can result in dry eyes. People with dry eyes may have minimal symptoms but often experience redness, irritation, a gritty sensation, and sensitivity to light. In severe cases, it can lead to blurred vision and inflammation of the cornea. Since it is a disease than can cause permanent damage to the eye surface early intervention is key.
Environmental and lifestyle factors contribute significantly to dry eyes. Extended exposure to wind, smoke, or dry air can worsen symptoms. And spending long hours in front of a computer or smartphone screen, which is a daily occurrence for most people, can severely impact dry eyes. These activities reduce blinking frequency, which is essential for spreading tears evenly over the eye surface. Hormonal changes, especially in postmeno- pausal women, and certain medications like antihistamines and antidepres- sants, can also contribute to a decrease in tear production.
Blepharitis, an inflammation of the eyelids, and Demodex mites, tiny parasites in hair follicles, can worsen dry eye symptoms by a9ecting the meibomian glands, which produce the oily layer of tears. Blocked or irritated glands lead to faster tear evaporation, causing dryness, redness, and discomfort. This condition can be related to common skin conditions such as rosacea. Proper eyelid hygiene, tea tree oil-based cleansers, and targeted treatments can help manage these issues and improve dry eye symptoms.
Treatment for dry eyes typically begins with addressing the underlying causes and making lifestyle changes. Lifestyle modifications like using a humidifier, taking breaks during screen use, and wearing protective eyewear in windy or sunny conditions can minimize symptoms. Maintaining good hydration and consuming a diet rich in omega-3 fatty acids has also been linked to improved tear production and eye health.
For mild cases, using over-the-counter artificial tears can provide immediate relief by supplementing natural tear production. These lubricating eye drops are available in preservative free formulations, which are particularly beneficial for individuals with sensitive eyes or those requiring frequent application.
For more persistent or severe cases, your dry eye specialist may recommend advanced therapies. One such option is prescription eye drops, such as cyclosporine (Restasis, Cequa, or Vevye) or lifitegrast (Xiidra), which work to reduce inflammation and stimulate tear production. Punctal plugs, tiny devices inserted into the tear ducts, can also help by preventing tears from draining away too quickly, allowing them to stay on the eye surface longer. Steroid eye drops may be used to quickly decrease inflammation while other therapies while other prescription treatments may take longer to be helpful. Varenicline (Tyrvaya) is a prescription nasal spray which can treat dry eye disease by stimulating tear production.
An innovative treatment for severe dry eye that we prescribe is autologous serum eye drops. These drops are created by drawing the patient’s blood, processing it to remove cells, and diluting the serum with saline. The result- ing solution contains growth factors, vitamins, and antibodies that closely mimic the composition of natural tears. Autologous serum drops promote healing of the cornea, reduce inflammation, and restore the natural balance of the tear film. This treatment is particularly beneficial for patients with chronic dry eye associated with conditions like Sjögren’s syndrome, graft- versus-host disease, or severe corneal damage and is generally well-tolerated when other therapies may be too irritating on damaged eye surfaces.
Treatments for blepharitis and Demodex focus on improving eyelid hygiene and reducing inflammation. Regular cleaning of the eyelid margins with warm compresses and gentle scrubs helps remove debris and unclog oil glands. For Demodex mites, tea tree oil-based cleansers or wipes are commonly used to eliminate the mites and reduce irritation. In more severe cases, doctors may prescribe antibiotics or anti-inflammatory eye drops or ointments to control infection and swelling. Advanced therapies, like in-o9ice deep lid cleaning procedures such as Blephex and Zest, can also provide relief when basic treatments aren’t enough.
OptiLight is the first FDA-approved intense pulsed light (IPL) treatment specifically designed for managing dry eye disease caused by meibomian gland dysfunction (MGD). This innovative therapy uses precise light pulses to target inflammation and improve the function of the meibomian glands, which produce the oily layer of the tear film. By reducing inflammation, unclogging glands, and addressing vascular abnormalities near the eyelid, OptiLight helps restore a healthier tear film and relieve dry eye symptoms.
The procedure is quick, non-invasive, and performed in our o9ice typically in 20 minutes or less. Most patients require a series of several sessions for optimal results. Similarly, devices like LipiFlow, TearCare, and iLux use heat and pressure to restore the function of the meibomian glands. For patients with evaporative dry eye caused by gland blockages, these therapies can significantly improve symptoms.
Preventing dry eyes often requires a multi-faceted approach tailored to individual needs. Regular eye exams are crucial for detecting underlying issues that may contribute to dry eyes, such as meibomian gland dysfunc- tion or blepharitis. Eye care professionals can offer personalized advice and recommend appropriate treatments based on the severity of symptoms and the root causes.
While dry eyes can be a chronic and frustrating condition, the wide range of available treatments and preventative measures ensures that most individuals can find relief. Dry eye syndrome is a complex condition that requires a multifaceted approach to treatment. Advances in medical technology and a deeper understanding of the condition continue to provide new options for improving quality of life.
Start now by taking a proactive approach to your dry eyes. Get regular eye exams and seek out an ophthalmologist who specializes in these advanced dry eye treatments sooner rather than later to improve your symptoms and prevent progression of the disease.